The Hidden Math of Prior Authorizations: How Insurers Game the System
Doug Jorgensen
February 9, 2025
Introduction: “Approved” Doesn’t Always Mean What You Think
Insurance companies love to quote numbers.
“90% of prior authorizations are approved.”
“Only 1 out of every 10 requests is denied.”
It sounds reassuring—until it’s your MRI, your medication, or your surgery that gets denied.
Here’s what they don’t tell you:
Those statistics are engineered to look good, not reflect reality.
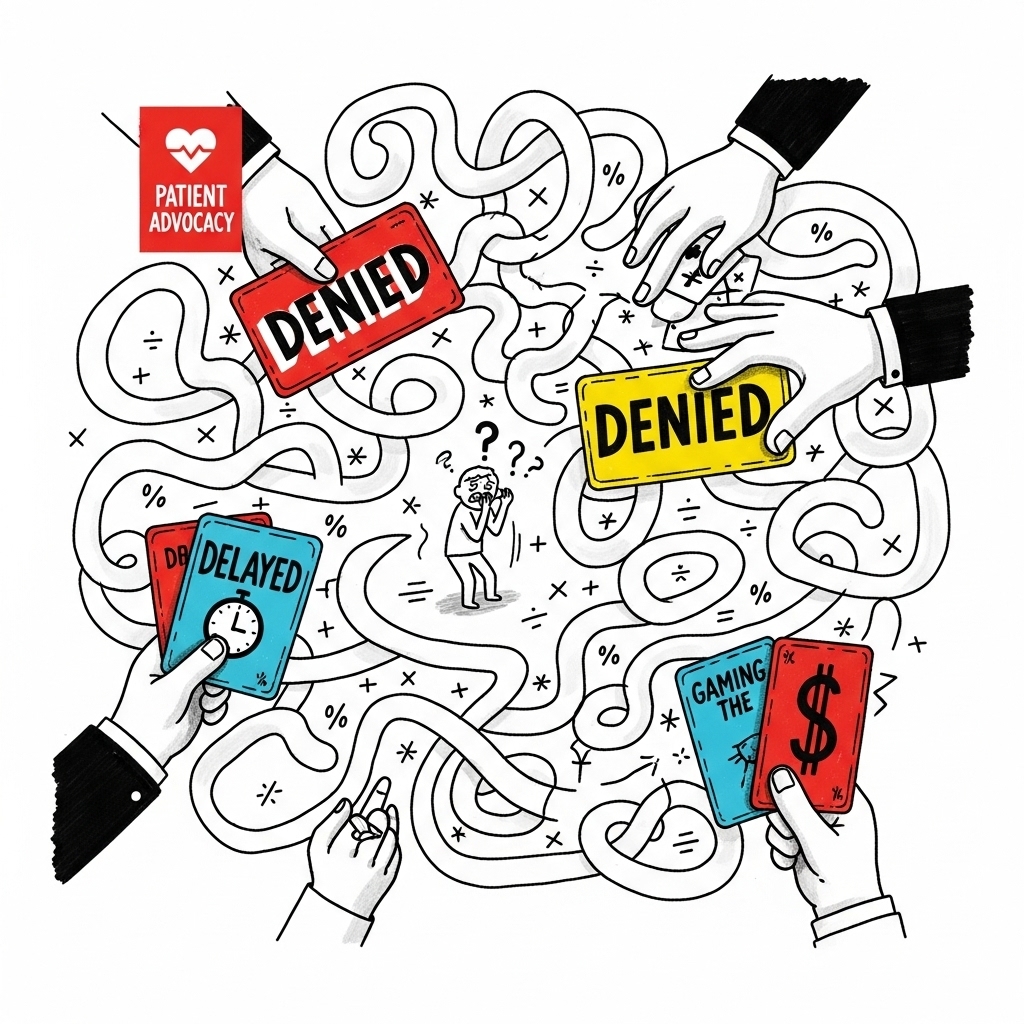
Behind the curtain, prior authorization is not just a clinical review.
It’s a calculated obstacle course—designed to slow down care, exhaust doctors, and push patients toward cheaper options or no care at all.
Let’s break down the math, the psychology, and the motive behind the game.
What Is Prior Authorization, Really?
Prior authorization (PA) is a process where your doctor must get approval from your insurance company before they can prescribe a certain medication, perform a procedure, or refer you to a specialist.
It’s pitched as a safety check—a way to ensure appropriate care. But make no mistake:
Prior authorization is a cost control mechanism.
It introduces friction. The more hoops patients and doctors have to jump through, the more likely they are to give up, delay care, or accept a cheaper, less effective alternative.
And that’s exactly the point.
The Real Numbers: Denial by Design
Let’s walk through how prior authorization really plays out in the system:
- 100 doctors submit a PA for the same MRI.
- 30 don’t complete the paperwork—either because it’s too time-consuming, unclear, or the process changes depending on the plan.
- Of the 70 who submit, 20 are denied outright.
- 10 of those 20 appeal.
- 6 get reversed on appeal.
The insurer now claims a 90% final approval rate—but in reality, only 56% of original patients got the test.
It’s not about what gets approved—it’s about what gets avoided.
That’s the hidden math.
Why It Works: The Psychology of Friction
Insurers know that time is limited—for both patients and providers.
- Patients get frustrated or scared.
- Doctors are overbooked, underpaid, and overwhelmed.
- Office staff don’t have hours to sit on hold or chase down faxes.
- Appeals take weeks—by which time the problem may have resolved, worsened, or become irrelevant.
The result?
Most people don’t appeal. Most doctors don’t push. And insurance companies quietly save billions by letting that inertia do their work for them.
But Wait—Didn’t They Say It’s “Medically Unnecessary”?
Yes. That’s often the reason cited for denial.
But here’s the catch:
The decision is usually made by someone who’s never met you, isn’t treating you, and sometimes isn’t even a licensed physician in your state or specialty.
In many cases, the person reviewing your case is:
- A nurse following a corporate checklist
- A physician working off of rigid, outdated criteria
- An algorithm trained to reject marginal requests based on cost
This isn’t medicine.
It’s spreadsheet-driven care rationing.
The Business Logic: Profits Through Attrition
Prior authorizations create a statistical firewall.
If even 30% of patients never make it past the initial denial, that’s 30% fewer procedures, drugs, or referrals the insurer has to pay for. Multiply that across millions of enrollees, and you’re looking at billions in reduced “medical losses.”
Every time you give up—your insurer makes money.
And every time you appeal and win? That’s not a system correction. That’s the exception they already budgeted for.
The Human Cost
While the math works well for insurers, the real-world cost is paid by:
- Patients who suffer from delayed diagnoses
- Doctors who get demoralized and burned out
- Hospitals that carry unpaid care costs
- Families who lose time, trust, and sometimes loved ones
This is not a hypothetical risk. It’s a documented national issue.
In fact, the American Medical Association has called for widespread prior authorization reform, citing patient harm and system inefficiency.
But change is slow.
So in the meantime, patients must learn to navigate—and challenge—the system.
How to Beat the Math: Patient Strategies
If you’ve been hit with a prior authorization denial, here’s what you can do:
1. Ask Your Provider to Appeal Immediately
Appeals often succeed—but only if filed.
2. Request a Peer-to-Peer Review
Your doctor can speak with a reviewer (ideally a peer in the same specialty) to argue the case.
3. Request Written Criteria
You have a right to see the exact criteria used to deny your care.
4. File a Complaint with the Bureau of Insurance
Let the state know this isn’t acceptable. Copy the insurer on the complaint.
5. Escalate with ERISA (if you’re on employer-based insurance)
As discussed in the previous article, ERISA gives you legal grounds to demand transparency.
6. Don’t Be Quiet
Use your voice—social media, employer HR, patient advocacy groups. Public pressure works.
Closing Thoughts: Don’t Be Fooled by the “Approval Rate” Spin
When insurers say, “Most prior authorizations are approved,” they’re not wrong—they’re just not telling the whole story.
They’re counting the patients who fought through the process.
Not the ones who got lost in it.
And that’s the goal: deny enough, delay enough, confuse enough—and save money quietly.
The only way to stop the cycle is to expose the math, understand the game, and refuse to accept “no” as the end of the conversation.
About the Author
Douglas J. Jorgensen, DO, CPC, FAAO, FACOFP
Dr. Doug is a nationally recognized regulatory expert, patient advocate, and medical consultant. With decades of experience in healthcare systems, audit defense, and physician policy, he works to expose the games insurers play—and empower patients and providers to push back.