How to Fight Back When Insurance Denies You Care: A Step-by-Step Guide
Doug Jorgensen
February 11, 2025
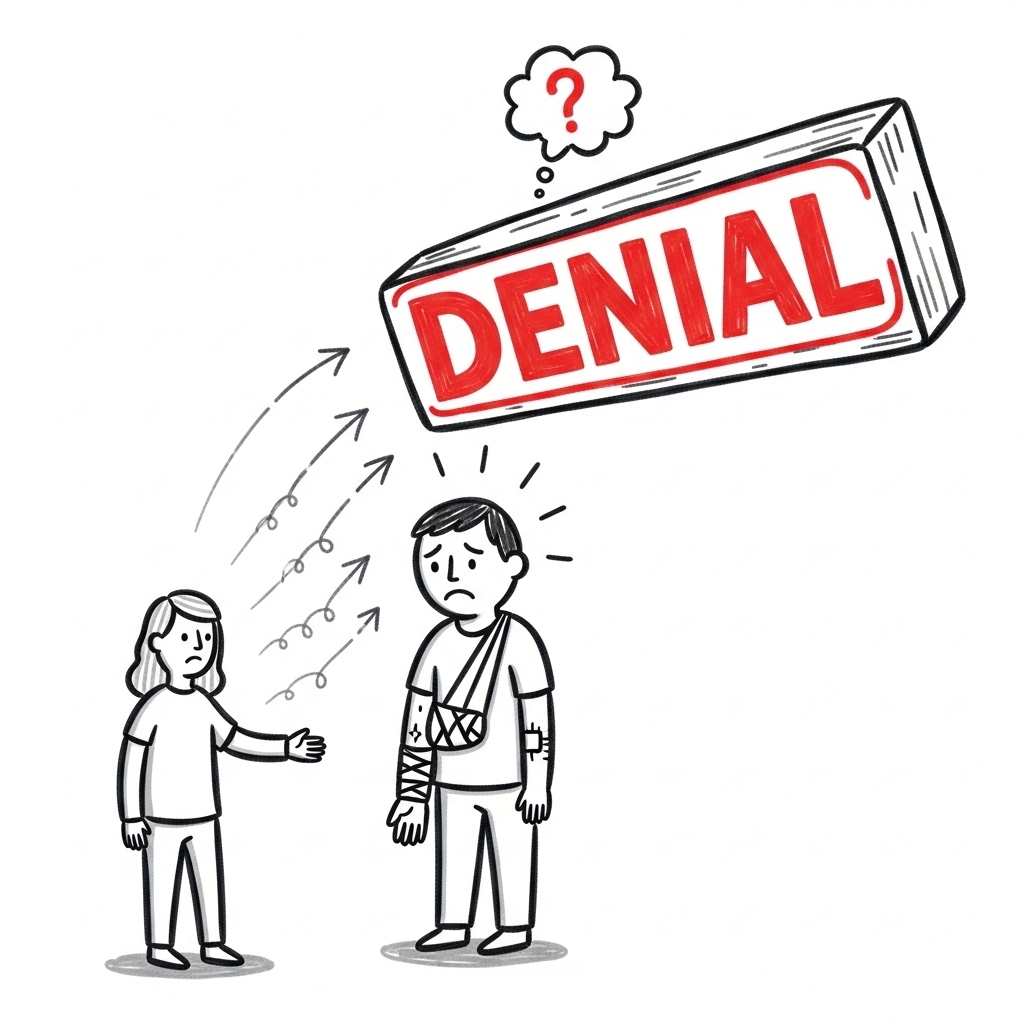
Introduction: Denied Doesn’t Mean Defeated
Every day, patients across the country are denied tests, procedures, medications, and referrals—often for care that their doctors consider medically necessary. If this has happened to you or someone you love, you probably felt frustrated, confused, and powerless.
But you are not powerless.
There are clear, actionable steps you can take to challenge the system—and in many cases, get the care you were originally denied. This guide outlines exactly how to do it, in the order that works best.
Step 1: Understand Why You Were Denied
Before you can fight a denial, you need to know exactly what you’re up against. Request a written explanation from your insurance company, which should include:
- The reason for the denial
- The clinical or policy criteria used
- Instructions for appeal
- Deadlines and forms you must follow
Pro Tip: Ask for the name and credentials of the reviewer, especially if it was a physician reviewer. You’re entitled to know who made the decision—and whether they’re qualified to do so.
Step 2: Involve Your Doctor Immediately
Your physician is a powerful ally in this process. Most denials can’t be overturned without clinical support from your provider.
Here’s what your doctor (or their office staff) can do:
- Request a peer-to-peer review with the insurance medical director
- Draft a medical necessity letter outlining why the treatment is required
- Submit supporting documentation (e.g., test results, prior treatments tried and failed)
- Help with the appeal paperwork
Important: Don’t assume your doctor will know the appeal timeline—you need to track the deadlines and keep the office updated.
Step 3: File an Internal Appeal
This is the first formal challenge to the insurance company’s decision. Your insurer is required to review your appeal in a timely manner—typically within 30 to 60 days.
To file:
- Follow the instructions on your denial letter
- Include your doctor’s documentation and any personal statements
- Keep a copy of everything you send
- Send it certified mail or use your insurer’s secure portal to track submission
Language to Use:
“This appeal is based on medical necessity as determined by my treating physician. I am requesting a formal reconsideration under the terms of my policy and under applicable federal law.”
Step 4: Escalate Through ERISA (If Applicable)
If you have employer-sponsored health insurance, your plan is likely governed by ERISA—a federal law that grants you specific rights.
Under ERISA:
- Your insurer must provide clear criteria for the denial
- They must give you access to all documentation used in their decision
- You have the right to an external review conducted by an independent third party
What to Say in Your Letter:
“As this plan is regulated under ERISA, I am formally requesting the documentation used to determine this denial, including all clinical criteria, reviewer information, and any internal guidelines applied.”
This tells the insurer you know the law—and that you’re serious.
Step 5: File a Complaint with the Bureau of Insurance
Every state has a Department or Bureau of Insurance that oversees insurers operating in your state. If you believe your denial is unjust, misleading, or harmful, you can file a formal complaint.
You can usually do this online.
Pro Tip: When you send future correspondence to the insurer, copy the Bureau of Insurance. This puts regulatory pressure on them and triggers internal compliance alerts.
Step 6: Use the Media—Including Social Media
Insurance companies care deeply about public perception. If you’ve been denied lifesaving or medically necessary care, share your story. You can:
- Post on social media platforms
- Tag the insurance company in your posts
- Contact local news outlets or patient advocacy groups
- Leave a review on public forums and employer portals
Be truthful and fact-based. Share exactly what happened and how it affected you or your family.
This isn’t just about attention—it’s about pressure. Insurance companies don’t want a PR problem, especially when it can be traced to a preventable denial.
Step 7: Consider Legal Support (If Needed)
If all appeals fail and the care was truly necessary, you may have grounds for legal action—especially under ERISA or if harm occurred due to delay or denial.
There are attorneys who specialize in:
- ERISA litigation
- Wrongful denial of benefits
- Malpractice resulting from delayed treatment
- Insurance bad faith claims
You may also qualify for pro bono support from patient advocacy organizations.
Step 8: Know That You’re Not Alone
Insurance denials are common—but that doesn’t make them acceptable. Thousands of patients every day are navigating this same fight. The difference between those who win and those who don’t often comes down to documentation, persistence, and knowledge.
Don’t let the system wear you down.
Don’t assume they’re right just because they said “no.”
And never forget: your health is worth the fight.
Closing Thoughts: You’re the Customer—But You Have to Act Like the Advocate
Your insurer works for you.
You pay the premiums. You trusted the plan.
But when that plan fails, it’s your job to push back.
This guide is your playbook. Use it. Share it. And when the next denial arrives—because there will be a next one—you’ll be ready.
About the Author
Douglas J. Jorgensen, DO, CPC, FAAO, FACOFP
Dr. Doug is a physician, federal policy advisor, and regulatory consultant with deep experience in healthcare systems, insurance disputes, and patient advocacy. His mission is simple: empower individuals with the knowledge they need to challenge a broken system and protect their right to care.